Doctors in European hospitals are having to wear top-to-bottom PPE and source vintage antibiotics from the 1960s to treat increasing numbers of Ukrainian soldiers who are presenting with antibiotic-resistant infections.
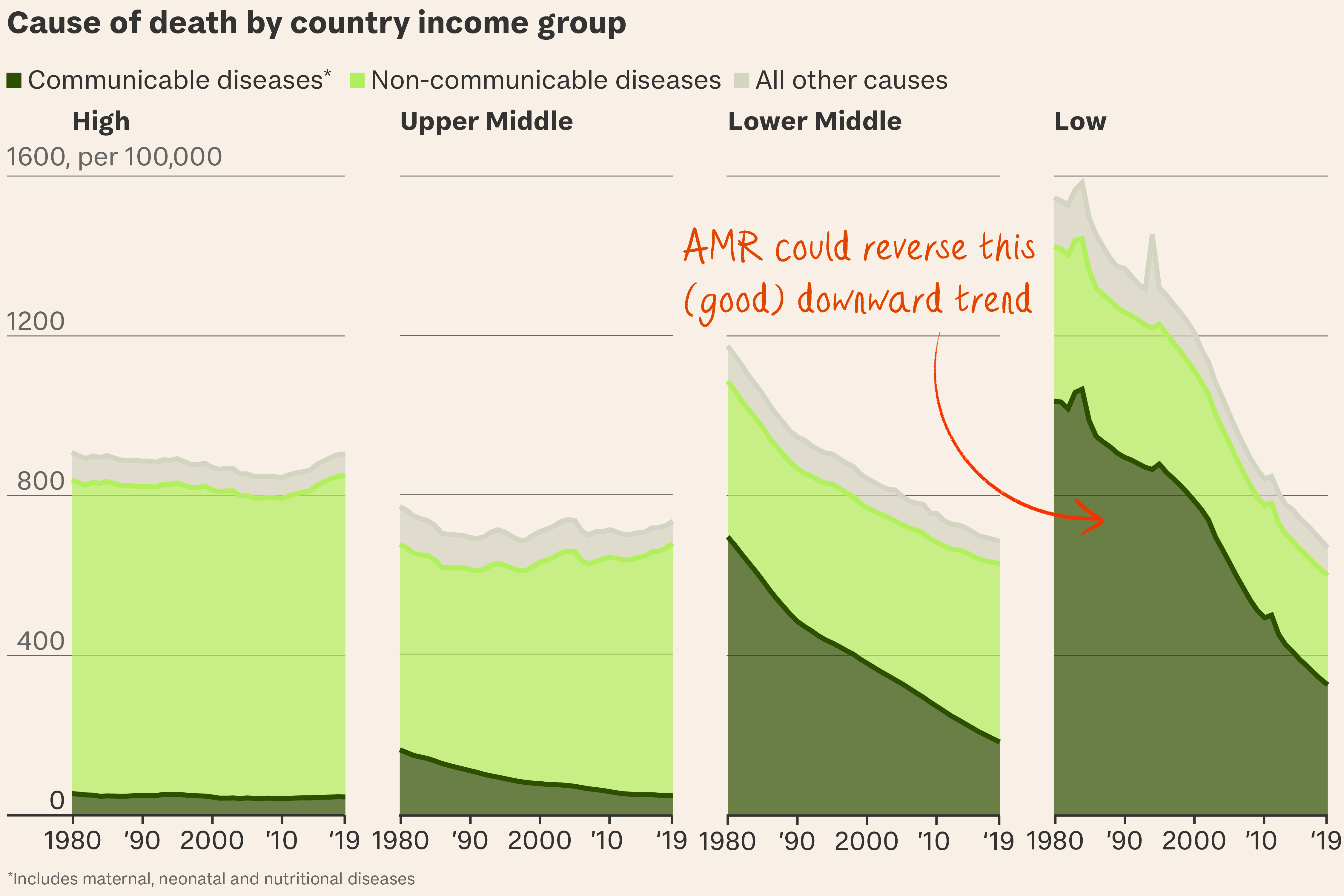
So what? This is just the speartip. The war in Ukraine is one of many catalysts fuelling a global public health crisis. Antibiotic resistance is the direct cause of 1.27 million deaths every year – more than annual deaths from malaria and HIV combined – and that number could rise to 10 million by 2050.
Told you so. Alexander Fleming, who discovered penicillin by accident almost a century ago, warned of antibiotic resistance in his 1945 Nobel lecture. It’s past time to heed his warning.
One in eight deaths worldwide was caused by bacterial infections in 2019. But humanity is losing its ability to treat them because of surging antimicrobial resistance (AMR), which occurs when misuse and overuse of antimicrobials – medicines used to prevent and treat infections – allows bacteria, viruses, fungi and parasites to evolve to no longer respond to them.
Left unchecked, AMR will
- undo decades of medical progress. Routine medical procedures like caesareans, chemotherapy and joint replacements will become riskier, and common infections untreatable. These include pneumonia, cholera, tuberculosis and infections from drug-resistant E. coli – of which there’s plenty in UK rivers, especially those near livestock farms (see below). Sewage dumping doesn't help.
- further burden already struggling healthcare systems, tipping an estimated 28 million people into poverty worldwide due to increased healthcare costs.
- lead to annual GDP losses of over $1 trillion by 2030, according to World Bank estimates. That’s the optimistic figure. In a “high AMR-impact scenario”, this rises to $3.4 trillion.
Sounds urgent. It is, but big pharma isn’t rushing to the rescue. No new classes of antibiotics have been brought to market in over 30 years. Pharmaceutical companies have little incentive to develop drugs by necessity destined for minimal use, when there are booming markets like those for weight loss drugs which generate big profits. Novo Nordisk is set to invest over $6 billion in Wegovy and Ozempic production this year alone.
Animal farm. Globally, 73 per cent of antimicrobials sold are used in livestock reared for food, often indiscriminately, preventively or to promote growth, which has led to a surge of AMR pathogens. Rife in the food chain, they then enter human microbiomes and make them more resistant to antimicrobials.
Say no to drugs. Humans aren’t doing themselves any favours. Most antibiotics are prescribed without diagnostic tests and handed out like lollipops. Shifting this habit of reaching for amoxicillin at the first sneeze is one of the biggest hurdles in combating AMR, according to Lord Ara Darzi, chair of the Fleming Initiative. He says “de-risking resistance” requires worldwide citizen engagement much like the climate crisis.
All or nothing. A fifth of drug-resistant infections occur in sub-Saharan Africa, where a "pandemic" of neonatal deaths is unfolding because of limited access to testing, vaccines and medication. Unequal global distribution of antimicrobials results in a lose-lose scenario for infection control. As Darzi puts it: "if you have access to antibiotics, you are misusing them. If you don't have access to antibiotics, you’re going to die of infection."
A germ of hope. Solutions involve pharma, farms and prudence:
- Infection prevention through access to clean water, improved sanitation and wider rollout of vaccines.
- Smarter diagnostics, allowing doctors to correctly identify and treat infections, minimising ‘blind’ prescriptions.
- Limiting antibiotic use in livestock through good husbandry rather than ‘bought-in’ infection control, especially in Asia, where antimicrobial use is highest.
- New antimicrobials. As existing antibiotics become ineffective, new ones are needed. 57 antibiotics and 40 non-traditional antibacterials are currently in clinical development – an R&D pipeline the WHO calls “insufficient”.
- Judicious use of existing antibiotics. Without this, even new ones will eventually become powerless.
What’s more… Ukrainian soldiers carry shame but not blame for bearing the bacterial brunt of trench warfare. But many of those being treated in German and Norwegian hospitals are racked with guilt and unable to express their gratitude. Medical teams have had to politely decline boxes of chocolates from soldiers, on account of infection control.